By Paul Sisson
Generally, fighting cancer is about delivering a relentless attack on the spreading disease, but a new approach explores the possible benefits of toggling therapy off and on like a light switch, allowing oncologists to more precisely control drug action and potential side effects.
A new trial just getting underway at Scripps Research Institute in La Jolla is using two novel medications in combination to create a sort of failsafe version of the “CAR” T-cell therapy that has proven effective at driving blood cancers such as lymphoma and leukemia into remission.
Concerns over potential toxicity and loss of potency have so far limited the applicability of these targeted white blood cells for treating other types of cancer outside the bloodstream. But Scripps researchers think the secret to better performance might be switchability, the capacity to “pulse” the action of T cells rather than simply having them do their work non-stop. The new trial, which recently enrolled its first patient, targets advanced breast cancer.
Travis Young, a chemical biologist and vice president of biologics at Scripps’ Calibr-Skaggs Institute for Innovative Medicine, said the team, led by chemist and Scripps Research CEO Peter Schultz, spent a dozen years designing a “platform” that has the ability to vary the intensity of treatment.
“Pete has described it as more of a light dimmer switch because you’re able to tune the precise amount of activity that you want,” Young said.
A T cell is a type of white blood cell that the human immune system can program to hunt down and destroy a wide range of threats from pathogens that have infected a person to the body’s own cells that have become cancerous, growing out of control, and damaging vital organs. The “CAR” in CAR T-cell therapy stands for Chimeric Antigen Receptor, a special piece of cellular equipment that scientists have learned to install in T cells harvested from a patient’s own blood.
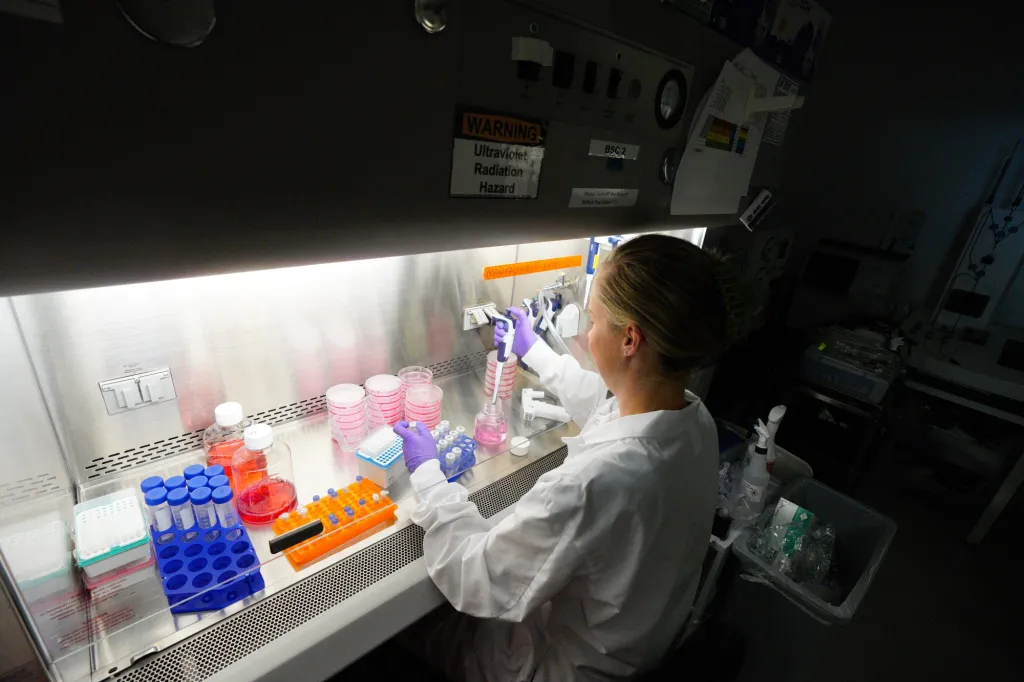
These cells are modified in a lab, encouraged to replicate themselves, and then re-infused back into a patient’s blood supply. The CAR is now along for the ride and is programmed to latch onto distinctive molecules called antigens on the surface of the patient’s specific kind of cancer.
But this CAR can end up building a little too much momentum in the body. Cancer cells, after all, are mutated versions of the body’s own cells, and these enhanced fighters can end up damaging healthy tissue more than their designers intend. Rapid multiplication of CAR T-cells in the body can also cause the release of proteins called cytokines which can, in too-high concentrations, become toxic. And, these cells do not have unlimited action. Like any cell, they cannot work forever killing cancer cells before exhausting their internal energy reserves, eventually losing their ability to keep fighting.
In all of these areas, Young said, having a CAR T-cell therapy that automatically turns itself off after a defined period of action seems like it could combat all of those drawbacks.
“Being able to switch the activity on and off allows us to give a pulse of therapy,” Young said. “It’s much different than running at full speed all the time, and the hypothesis we’re looking to test now is, if we’re able to pulse CAR T-cell therapy, are we able to overcome some of the barriers that we’ve never been able to overcome before?”
The key to making T cells switchable is in combining something that lasts a long time with something that is very short-lived.
Studies have shown that T cells can live in the body for many months, and those that the Calibr team designed have a sort of generic receptor, one that is not designed to bind directly with any cancer cell. Rather, the CARs on these cells are designed to function something like the chuck on an electric drill. Just as a drill’s parallel clamping jaws are designed to spin many different types of bits, the receptors on Calibr’s switchable T cells are able to bind with any molecule that corresponds to the shape of their custom CAR.
This allows a second drug molecule, one designed with a cancer target on one end and an opposite end that binds with the generic receptor to snap in place. And switchable T cells are made to attack cancer cells only if they are connected to one of these special targeting molecules. In this case, breast cancer antigen targets are made by AbbVie, a Chicago-based international pharmaceutical company.
But, unlike metal drill bits, which generally last for years, these enabling molecules are designed to degrade very quickly, falling apart within a few days at most. When they disintegrate, the switchable T cells they were attached to stop working automatically. All it takes to get them working again is to infuse a patient with a fresh dose and another period of T cell cancer hunting begins. If the genetic signature of a patient’s cancer cells has changed from the previous dose, a new target, or multiple targets, could be specified with a new dose.
This feature, essentially a failsafe, Young explained, allows CAR cells to take a break, which can be useful in terms of keeping cytokine production from getting out of control and from becoming exhausted from working too long without time to rejuvenate. These switchable cells, Young adds, are able to multiply themselves much more extensively than previous CAR T cells have in the past. This ability was shown in a study that used switchable CAR T cells to target disregulated B cells, a type of white blood cell, in mice.
“We have shown in our trials for B cell malignancies that we can get up to tenfold the expansion of CAR T cells, and being able to just produce more numbers, while also being able to give them a rest, those are both reasons why we think we’re going to be effective in solid tumors,” Young said.
Christine Brown, a molecular biologist and director of the T Cell Therapeutics Research Laboratory at City of Hope cancer center based in Duarte, said the approach does appear to be novel. Controlling T-cell activity, Brown said, is a growing topic of interest with various approaches under investigation, from using “genetic circuits” to modulate responses to “suicide switches” that cause T-cells to self-destruct on command if they get out of hand.
Brown said that City of Hope is working on a similar technology using a different mechanism that it hopes to have in clinic next year.
She said that the idea of being able to turn T-cells on and have them turn themselves off after a predictable period of action could indeed allow for more gradual and prolonged courses of therapy.
“The idea of having more options for how much you dose, how long yo dose, I’m very interested to see what comes out of these clinical studies,” Brown said. “I think there is potential and excitement for the possible utility of this kind of approach, but these ideas have not yet really been clinically explored nearly as much as hard-wired CARs.
“That’s why I think this is exciting, because it’s an area where there is still a lot to learn.”
Scripps hopes to enroll 20 patients in its phase 1 clinical trial for switchable CAR T cells in patients with advanced or metastatic breast cancer who have no other options. Study sites include UC San Diego Moores Cancer Center, and centers at Indiana University and Roswell Park Cancer Center in Buffalo, N.Y.
But Calibr is already working on the next generation of its switchable technology. Young said the next idea is to find a way to insert the genetic instructions to make T cells switchable without taking them out of the body.